Contents
- Healthcare Infrastructure
- NGOs and Initiatives
- JF Ajmera Rotary Netra Rugnalaya & the Rotary Club
- Annapurna
- Graphs
- Healthcare Facilities and Services
- A. Patients in In-Patients Department
- B. Patients in Outpatients Department
- C. Outpatient-to-Inpatient Ratio
- D. Operations Conducted
- E. Hysterectomies Performed
- F. Share of Households with Access to Health Amenities
- Morbidity and Mortality
- A. Reported Infant Deaths
- B. Select Causes of Infant Death
- C. Number of Children Diseased
- D. Population with High Blood Sugar
- E. Population with Very High Blood Sugar
- F. Population with Mildly Elevated Blood Pressure
- G. Population with Moderately or Severely High Hypertension
- H. Women Examined for Cancer
- I. Alcohol and Tobacco Consumption
- Maternal and Newborn Health
- A. Reported Deliveries
- B. Institutional Births: Public vs Private
- C. Home Births: Skilled vs Non-Skilled Attendants
- D. Live Birth Rate
- E. Still Birth Rate
- F. Maternal Deaths
- G. C-section Deliveries: Public vs Private
- H. Institutional Deliveries through C-Section
- I. Deliveries through C-Section: Public vs Private Facilities
- J. Reported Abortions
- K. Medical Terminations of Pregnancy: Public vs Private
- L. MTPs in Public Institutions before and after 12 Weeks
- M. Average Out of Pocket Expenditure per Delivery in Public Health Facilities
- N. Registrations for Antenatal Care
- O. Antenatal Care Registrations Done in First Trimester
- P. Iron Folic Acid Consumption Among Pregnant Women
- Q. Access to Postnatal Care from Health Personnel Within 2 Days of Delivery
- R. Children Breastfed within One Hour of Birth
- T. Children (6-23 months) Receiving an Adequate Diet
- T. Sex Ratio at Birth
- U. Births Registered with Civil Authority
- V. Institutional Deliveries through C-section
- W. C-section Deliveries: Public vs Private
- Family Planning
- A. Population Using Family Planning Methods
- B. Usage Rate of Select Family Planning Methods
- C. Sterilizations Conducted (Public vs Private Facilities)
- D. Vasectomies
- E. Tubectomies
- F. Contraceptives Distributed
- G. IUD Insertions: Public vs Private
- H. Female Sterilization Rate
- I. Women’s Unmet Need for Family Planning
- Immunization
- A. Infants Given the Oral Polio Vaccine
- C. Infants Given the Bacillus Calmette Guerin (BCG) Vaccine
- C. Infants Given Hepatitis Vaccine (Birth Dose)
- D. Infants Given the Pentavalent Vaccines
- E. Infants Given the Measles or Measles Rubella Vaccines
- F. Infants Given the Rotavirus Vaccines
- G. Fully Immunized Children
- H. Adverse Effects of Immunization
- I. Percentage of Children Fully Immunized
- J. Vaccination Rate (Children Aged 12 to 23 months)
- K. Children Primarily Vaccinated in (Public vs Private Health Facilities)
- Nutrition
- A. Children with Nutritional Deficits or Excess
- B. Population Overweight or Obese
- C. Population with Low BMI
- D. Prevalence of Anaemia
- E. Moderately Anaemic Women
- F. Women with Severe Anaemia being Treated at an Institution
- Sources
DHARASHIV
Health
Last updated on 26 July 2025. Help us improve the information on this page by clicking on suggest edits or writing to us.
Dharashiv’s healthcare landscape, like many other regions across India, is shaped by a mix of indigenous and Western medical practices. For centuries, indigenous knowledge and treatments provided by practitioners such as hakims and vaidyas have formed the foundation of healthcare in the region. This long-standing relationship between communities and their natural environment played a key role in shaping the district’s early medical traditions. Over time, its landscape has gradually evolved with the introduction and expansion of more specialised medical services.
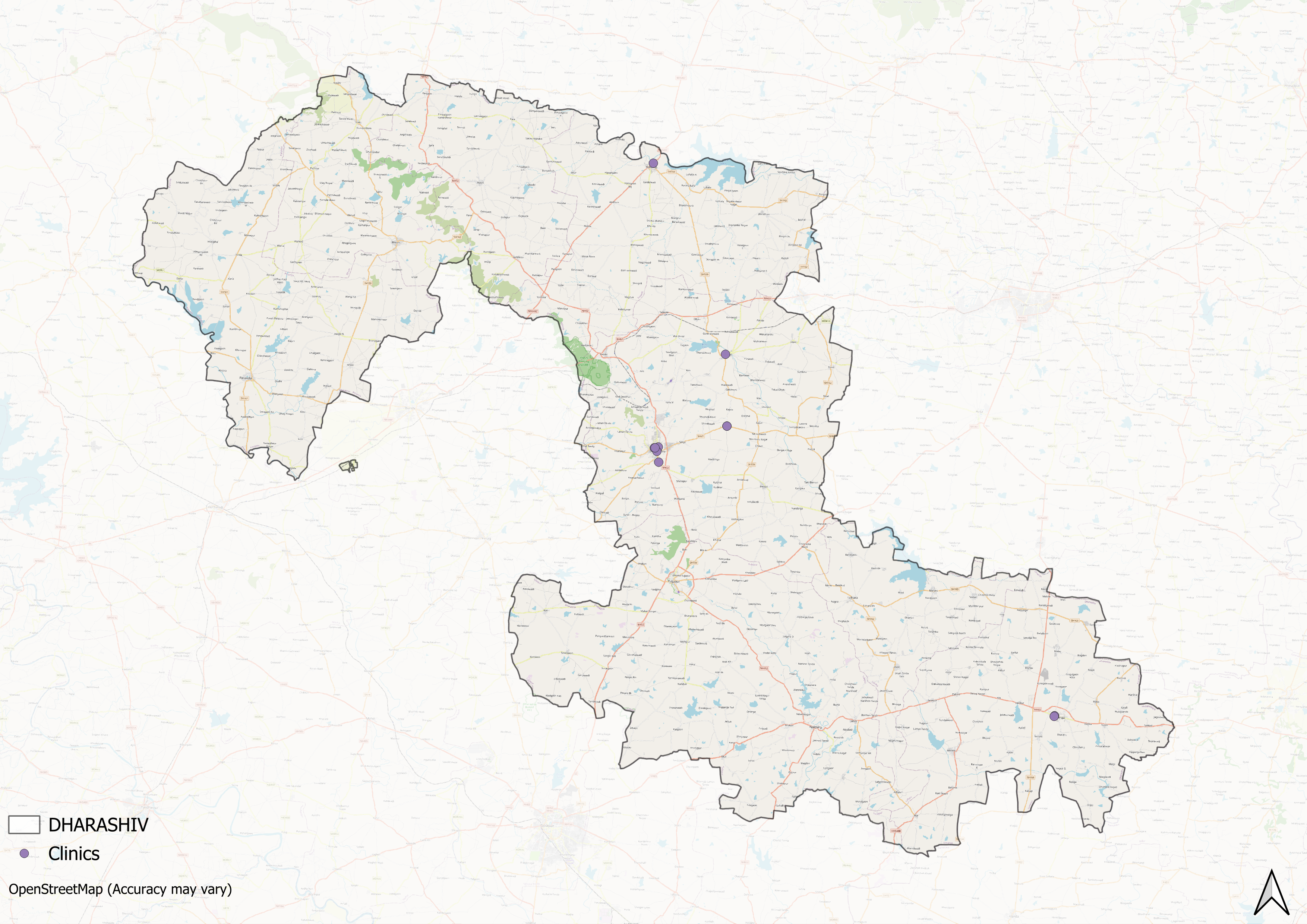
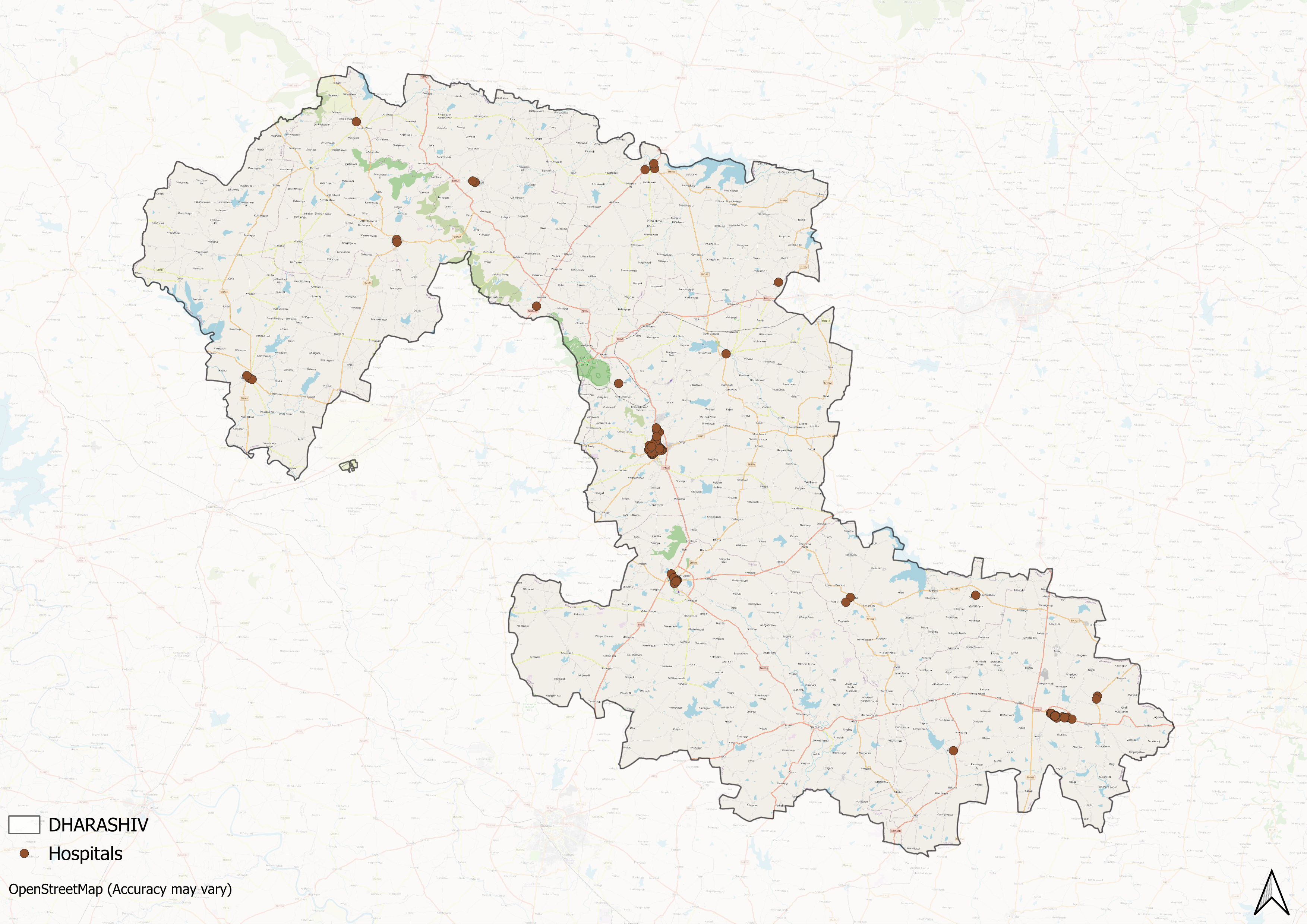
Healthcare Infrastructure
Much like other regions in India, Dharashiv’s healthcare infrastructure follows a multi-tiered system that involves both public and private sectors. The public healthcare system is structured into primary, secondary, and tertiary levels. Primary care is provided through Sub Centres and Primary Health Centres (PHCs), secondary care is managed by Community Health Centres (CHCs) and Sub-District hospitals, while tertiary care, the highest level, is delivered through Medical Colleges and District Hospitals.
Supporting this structure is a network of Accredited Social Health Activists (ASHAs) who, as described by the National Health Mission, serve as “an interface between the community and the public health system.” Over time, this multi-layered healthcare model has been continuously shaped and refined by national healthcare policies and reforms to provide universal health coverage across regions.
The General Hospital has served for decades as the main government-run facility in the district. Its earlier units included radiology and pathology services from the 20th century, showing the presence of basic diagnostic and treatment departments. At present, Dharashiv’s main public healthcare facilities include the District Women’s Hospital and the Civil Hospital, which provide medical services to the local population.
![District Hospital[1]](/media/statistic/images/maharashtra/dharashiv/health/district-hospital1-f7e44d1e.png)
In recent years, the district’s healthcare system has expanded through work by local trusts, non-governmental organisations, government measures, and individual practitioners. In 2024, the Asian Development Bank (ADB) approved funding of Rs 4,000 crore for upgrades to health facilities across Maharashtra, with an initial tranche of Rs 1,200 crore already allocated. A portion of this funding is planned for the construction of a new 500-bed hospital in Dharashiv to add to the district’s existing medical infrastructure.
NGOs and Initiatives
The determinants of health and health outcomes, as the World Health Organisation (WHO) elaborates, are not solely shaped by more than just medical factors and healthcare services. The organisation uses the term “social determinants of health (SDH)” to refer to the “non-medical factors that influence health outcomes.” These non-medical factors can be sanitation, nutrition, community well-being, or, as the WHO outlines, “income and social protection,” “food security,” access to quality healthcare, and more.
While there have been ongoing efforts to strengthen Dharashiv district’s healthcare infrastructure, certain areas still face challenges, particularly in addressing these broader health determinants. In response, non-governmental organisations have emerged as vital partners, working alongside public health systems to develop innovative, grassroots-level approaches that bridge these gaps.
JF Ajmera Rotary Netra Rugnalaya & the Rotary Club
One such initiative is the JF Ajmera Rotary Netra Rugnalaya, which was established by a charitable trust to expand access to eye care services in Dharashiv. The facility was set up under the leadership of Ravindra Salunke and the Rotary Club of Dharashiv. Work on the hospital began before 2005, following a survey that indicated there were no private hospitals within a 150 km radius equipped to treat eye diseases.
![JF Ajmera Rotary Netra Rugnalaya[2]](/media/statistic/images/maharashtra/dharashiv/health/jf-ajmera-rotary-netra-rugnalaya2-b7aa3e7e.png)
To raise funds for the hospital, the Rotary Club used local donations and crowdfunding. Recruiting qualified medical professionals was an early challenge due to Dharashiv’s location, so a training programme for paramedics was introduced to maintain essential services. The hospital operates on a mixed model, combining free services with a limited number of paid treatments to remain financially viable.
Annapurna
Annapurna is a local food assistance programme set up to address food insecurity in parts of Dharashiv district affected by repeated droughts and limited economic resources. The initiative distributes cooked meals to families who face difficulties in accessing regular nutrition.
During the COVID-19 lockdown, the programme adjusted its operations to deliver daily tiffins to around 700 people, including migrant workers. Annapurna continues to provide food support in the district, particularly during periods of economic strain.
Graphs
Healthcare Facilities and Services
Morbidity and Mortality
Maternal and Newborn Health
Family Planning
Immunization
Nutrition
Sources
Construction Week Online. 2024. ADB’s ₹4,000 Cr Investment to Boost Maharashtra’s Healthcare Facilities. Construction Week Online, India.https://www.constructionweekonline.in/business/adbs-rs-4000-cr-investment-to-boost-maharashtras-healthcare-facilitieshttps://www.constructionweekonline.in/busine…
George, Mathew. 2023. The Real Purpose of the Medical College.The Hindu.https://www.thehindu.com/opinion/op-ed/the-real-purpose-of-the-medical-college/article67232008.ecehttps://www.thehindu.com/opinion/op-ed/the-r…
M Choksi, B. Patil et al. 2016.Health systems in India.Vol 36 (Suppl 3).Journal of Perinatology.https://pmc.ncbi.nlm.nih.gov/articles/PMC5144115/https://pmc.ncbi.nlm.nih.gov/articles/PMC514…
Maharashtra State Gazetteers. 1972. Dharashiv (Osmanabad) District Gazetteer: Medical Facilities. Gazetteer Department, Government of Maharashtra, Mumbai.
National Health Mission (NHM). n.d. "About Accredited Social Health Activist (ASHA)." National Health Mission, India.https://nhm.gov.in/index1.php?lang=1&level=1&sublinkid=150&lid=226#:~:text=One%20of%20the%20key%20components,performing%20her%20spelled%20out%20roles.https://nhm.gov.in/index1.php?lang=1&level=1…
Nitnaware, Himanshu. 2020. Atul Ajmera’s Annapurna Initiative: Free Food for Needy Patients in Osmanabad. The Better India, India.https://thebetterindia.com/241410/atul-ajmera-annapurna-osmanabad-free-food-civil-hospital-patient-kin-needy-drought-inspiring-him16/https://thebetterindia.com/241410/atul-ajmer…
The Logical Indian. 2020. Providing Vision to the Needy: A Healthcare Initiative. The Logical Indian, India.https://thelogicalindian.com/health/providing-vision-to-the-needy-24798https://thelogicalindian.com/health/providin…
World HealthOrganisation(WHO). Social Determinants of Health. World HealthOrganisation.https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1https://www.who.int/health-topics/social-det…
Last updated on 26 July 2025. Help us improve the information on this page by clicking on suggest edits or writing to us.