Contents
- Healthcare Infrastructure
- Age-Old Practices & Remedies
- Karmaveer Vyankatrao Tanaji Randhir Ayurveda College
- Palu Utarne
- Sherry Utarne
- Treatment of Injuries
- Vahvam Zaptayana
- Moternu
- Johor Utarane
- Graphs
- Healthcare Facilities and Services
- A. Public and Govt-Aided Medical Facilities
- B. Private Healthcare Facilities
- C. Approved vs Working Anganwadi
- D. Anganwadi Building Types
- E. Anganwadi Workers
- F. Patients in In-Patients Department
- G. Patients in Outpatients Department
- H. Outpatient-to-Inpatient Ratio
- I. Patients Treated in Public Facilities
- J. Operations Conducted
- K. Hysterectomies Performed
- L. Share of Households with Access to Health Amenities
- Morbidity and Mortality
- A. Reported Deaths
- B. Cause of Death
- C. Reported Child and Infant Deaths
- D. Reported Infant Deaths
- E. Select Causes of Infant Death
- F. Number of Children Diseased
- G. Population with High Blood Sugar
- H. Population with Very High Blood Sugar
- I. Population with Mildly Elevated Blood Pressure
- J. Population with Moderately or Severely High Hypertension
- K. Women Examined for Cancer
- L. Alcohol and Tobacco Consumption
- Maternal and Newborn Health
- A. Reported Deliveries
- B. Institutional Births: Public vs Private
- C. Home Births: Skilled vs Non-Skilled Attendants
- D. Live Birth Rate
- E. Still Birth Rate
- F. Maternal Deaths
- G. Registered Births
- H. C-section Deliveries: Public vs Private
- I. Institutional Deliveries through C-Section
- J. Deliveries through C-Section: Public vs Private Facilities
- K. Reported Abortions
- L. Medical Terminations of Pregnancy: Public vs Private
- M. MTPs in Public Institutions before and after 12 Weeks
- N. Average Out of Pocket Expenditure per Delivery in Public Health Facilities
- O. Registrations for Antenatal Care
- P. Antenatal Care Registrations Done in First Trimester
- Q. Iron Folic Acid Consumption Among Pregnant Women
- R. Access to Postnatal Care from Health Personnel Within 2 Days of Delivery
- S. Children Breastfed within One Hour of Birth
- T. Children (6-23 months) Receiving an Adequate Diet
- U. Sex Ratio at Birth
- V. Births Registered with Civil Authority
- W. Institutional Deliveries through C-section
- X. C-section Deliveries: Public vs Private
- Family Planning
- A. Population Using Family Planning Methods
- B. Usage Rate of Select Family Planning Methods
- C. Sterilizations Conducted (Public vs Private Facilities)
- D. Vasectomies
- E. Tubectomies
- F. Contraceptives Distributed
- G. IUD Insertions: Public vs Private
- H. Female Sterilization Rate
- I. Women’s Unmet Need for Family Planning
- J. Fertile Couples in Family Welfare Programs
- K. Family Welfare Centers
- L. Progress of Family Welfare Programs
- Immunization
- A. Vaccinations under the Maternal and Childcare Program
- B. Infants Given the Oral Polio Vaccine
- C. Infants Given the Bacillus Calmette Guerin (BCG) Vaccine
- D. Infants Given Hepatitis Vaccine (Birth Dose)
- E. Infants Given the Pentavalent Vaccines
- F. Infants Given the Measles or Measles Rubella Vaccines
- G. Infants Given the Rotavirus Vaccines
- H. Fully Immunized Children
- I. Adverse Effects of Immunization
- J. Percentage of Children Fully Immunized
- K. Vaccination Rate (Children Aged 12 to 23 months)
- L. Children Primarily Vaccinated in (Public vs Private Health Facilities)
- Nutrition
- A. Children with Nutritional Deficits or Excess
- B. Population Overweight or Obese
- C. Population with Low BMI
- D. Prevalence of Anaemia
- E. Moderately Anaemic Women
- F. Women with Severe Anaemia being Treated at an Institution
- G. Malnourishment Among Infants in Anganwadis
- Sources
DHULE
Health
Last updated on 26 July 2025. Help us improve the information on this page by clicking on suggest edits or writing to us.
Dhule’s healthcare landscape, like many other regions across India, is shaped by a mix of indigenous and Western medical practices. For centuries, indigenous knowledge and treatments provided by practitioners such as hakims and vaidyas have formed the foundation of healthcare in the region. Notably, Dhule lies in a region with varied terrain shaped by the Satpura mountain ranges. Many parts of the district are home to indigenous communities who have lived in close connection with forests, hills, and local plant resources for generations.
This close link with the natural environment influenced the way people treated illnesses, relying on plants, herbs, and local remedies passed down through families and community healers. Much of Dhule’s formal healthcare infrastructure began to take shape under colonial rule with the establishment of the Civil Hospital in 1825. Over the years, the region has witnessed several significant developments in healthcare delivery.
Healthcare Infrastructure
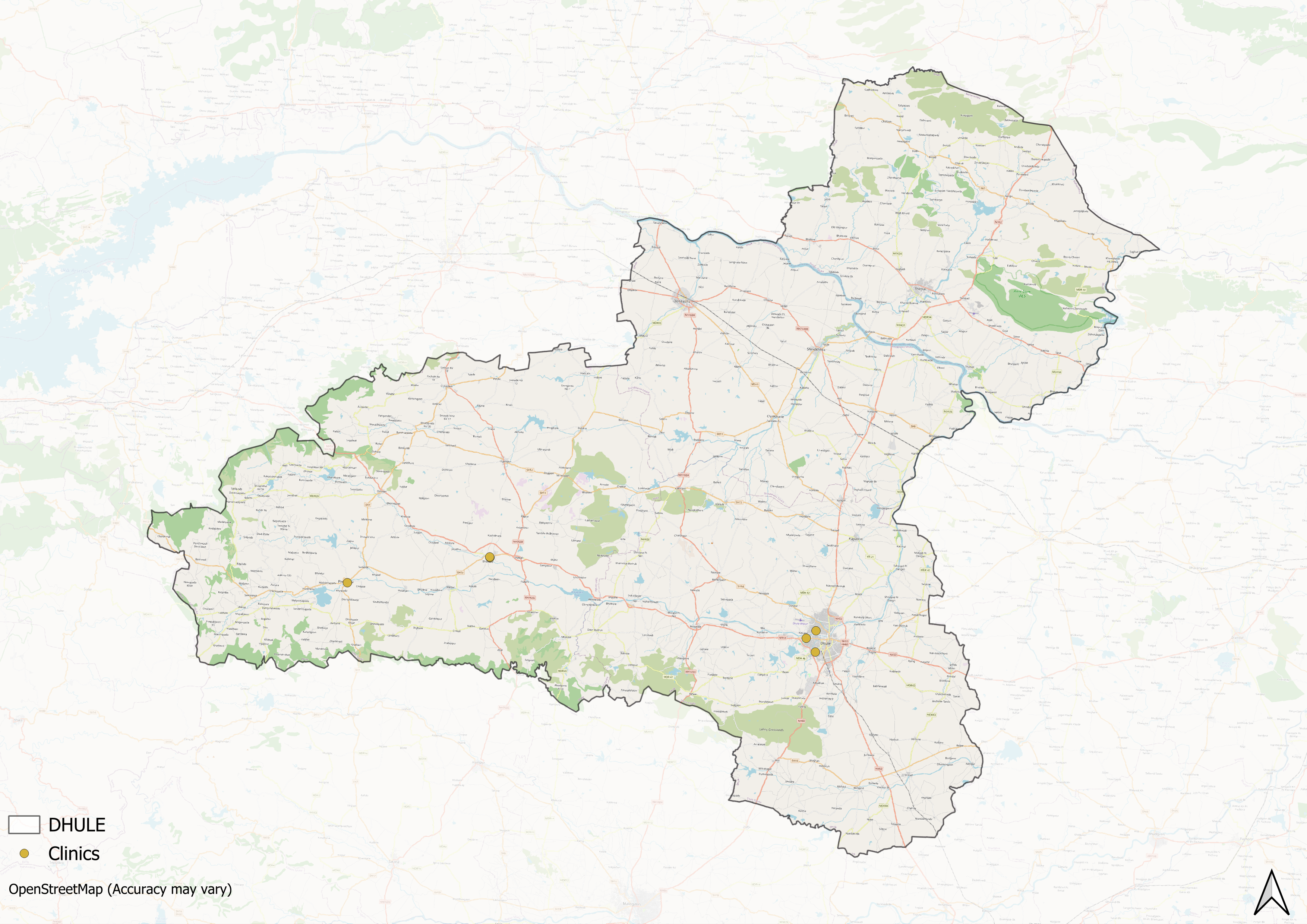
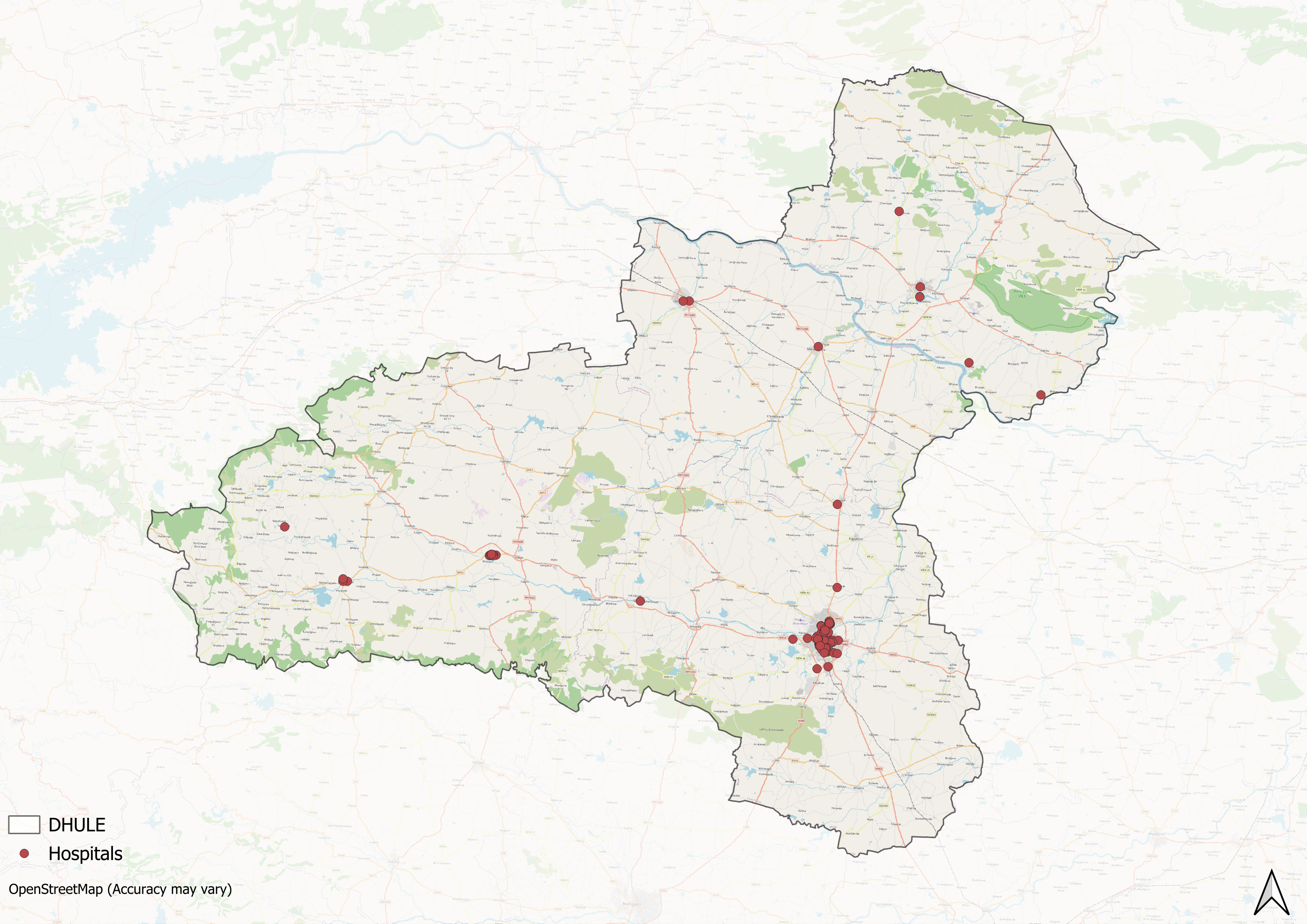
Similar to other regions in India, Dhule’s healthcare infrastructure follows a multi-tiered system that involves both public and private sectors. The public healthcare system is structured into primary, secondary, and tertiary levels. Primary care is provided through Sub Centres and Primary Health Centres (PHCs), secondary care is managed by Community Health Centres (CHCs) and Sub-District hospitals. However, tertiary care, the highest level, is delivered through Medical Colleges and District Hospitals.
Supporting this structure is a network of Accredited Social Health Activists (ASHAs) who, as described by the National Health Mission, serve as “an interface between the community and the public health system.” Over time, this multi-layered healthcare model has been continuously shaped and refined by national healthcare policies and reforms to improve universal health coverage across regions.
Dhule’s formal healthcare system, like that of much of India, traces its foundations to the colonial era. As Rama Baru (1999) on, the beginnings of this system, allopathic medicine was introduced by the British in the mid-18th century, chiefly to serve their civilian and military establishments. Dhule formed part of the British administrative and military framework in the region. One of its earliest and most enduring institutions was the Civil Hospital, established in 1825 to attend to the medical needs of local communities and stationed troops.
In 1874, as part of broader administrative changes, the hospital was shifted to a new military hospital building, following the withdrawal of regular troops from Khandesh. This relocation hints at an adjustment in the hospital’s role, perhaps to continue serving residual military personnel or to repurpose existing infrastructure for the local population’s benefit.
Over time, Dhule’s healthcare landscape continued to change. The public health system expanded gradually with the addition of more government-run facilities. In the 20th and 21st centuries, private hospitals also began to appear in the district, often established by local trusts, non-governmental organisations, and individual community efforts. However, similar to broader patterns that can be seen across India, the district’s healthcare infrastructure has developed unevenly across geographic lines. While urban areas experienced substantial growth in private healthcare facilities, rural regions remained predominantly served by government-run hospitals, with fewer private facilities (see statistics below).
Age-Old Practices & Remedies
Historically, before the advent of Western healthcare systems or the three-tiered healthcare infrastructure that exists today, people in the district relied on and made use of indigenous knowledge and medicine for their well-being. When it comes to healthcare in India, which has long been characterized by a pluralistic health tradition. Among the many medicine systems that have a long history in India and Dhule, as locals say, are Ayurveda and Unani.
Karmaveer Vyankatrao Tanaji Randhir Ayurveda College
In Dhule district, one significant institutional step towards preserving and teaching Ayurveda came in 1972, when Late Karmaveer Vyankatrao Tanaji Randhir founded the Karmaveer Vyankatrao Tanaji Randhir Ayurveda College. Located in Boradi, a remote area with limited infrastructure at the time, the college was set up to offer Ayurvedic education and medical services to rural and tribal communities. The college provides training through 14 specialised departments, covering fields such as Rasa-Shastra and Rognidan.

Alongside education, the college is also known locally for its hospital services. Lilai Ayurved Hospital, attached to the college, is recognised for its treatment of various diseases using Ayurvedic methods, with a particular reputation for treating paralysis.

Traditional Healers and Local Practices
Outside formal institutions, traditional medicine has long played an important role in daily life, especially among indigenous communities. In many padas (hamlets), people depended on vaidyas (healers) who diagnosed illnesses through techniques such as nadi pariksha (pulse reading). Rituals like tying a Ganda Dora (sacred thread) were believed to aid healing. The Pawra community in Dhule is especially known for its deep knowledge of local plants and ethnomedicinal practices, which are closely tied to their forest environment and way of life.
Palu Utarne
Palu Utarne involves using Palu (the leaves of the Apta tree) to treat illnesses in the presence of devtas and devis who are entwined with nature. This ritual is commonly performed by the community for ailments like headaches or prolonged fevers. The procedure involves collecting various items, such as Palu, red eye chili, thick salt, and neem sticks, which are placed in a flour sieve and rotated seven times over the patient's body while chanting a mantra. The used leaves are then placed in boiling water.
Once the water turns red, the leaves are thrown in the middle of a road. This act carried the belief that anyone or anything crossing this line would take on the disease. This belief was thought to help the patient recover. If there was no improvement, the process was repeated after a day or two, with the same leaves being burned under the bed.
![Palu[1]](/media/statistic/images/maharashtra/dhule/health/palu1-a44886a9.png)
During this procedure, the sick person would lie on a cot covered with a sheet to trap the smoke. This method, known as "washing," was believed to purify and heal the patient. If the condition persisted despite this treatment, the “Budva” (traditional healer) would be consulted for further diagnosis and care.
Sherry Utarne
In the Pawra community, Sherry means fever. In the past, transportation challenges often prevented people from reaching hospitals, so they turned to a Budva for treatment. Different types of Budva exist, each with specific methods and rituals for addressing fevers and other illnesses. Variations in pronunciation, such as Budva, Bodvu, and Buduvu, reflect local dialects. Treatments sometimes involved facing the rising sun, marking the patient’s shadow with an iron knife, or using natural items such as seeds or animal remains.
Treatment of Injuries
Traditional methods are also used to treat physical injuries, such as swelling or broken bones. Swelling is treated by boiling leaves from the Awvi tree and applying them to the affected area overnight. Broken limbs are immobilised with bamboo splints secured by rope made from the bhend plant. To help bone healing, a piece of the jointed trunk of a vine known locally as Hatjulam is consumed, as it is believed to support the repair and joining of broken bones.
Vahvam Zaptayana
In the Dhule district, certain seasonal winds known as Bhutya are believed to affect health. These high winds, common at the start of summer and during the monsoon season in hilly areas, are thought by the community to carry harmful effects that can cause illness if encountered directly. The Bhutya winds are described as having different forms and sounds, which are said to vary by time of day and may influence the severity of their effects.
Exposure to these winds is believed to cause symptoms such as vomiting, fever, and headache. In severe cases, such illnesses could be fatal. People who fell sick after coming into contact with these winds were referred to as Vahvam Zaptaigya. When this occurred, families would consult a Budva (traditional healer) to perform rituals intended to remove the effects of the wind and restore health.
Moternu
Moternu is a traditional method used to treat various injuries and conditions such as wounds, burns, tumours, and stomachaches. Diagnosis is carried out by a Budva, who uses a mix of materials including women’s hair, ash, neem leaves, and village chicken eggs. A hair rope, known as a Selari, is tied around the injured area to conceal it and prevent the spread of the injury.
Johor Utarane
In the Pawra community, Johor refers to animal poison. Traditional treatments for bites from snakes, scorpions, and other poisonous creatures include the use of neem leaves and fire ash, along with rituals meant to draw out or neutralise the poison. Locals say that these methods are still practised in some areas where access to medical facilities may be limited.
Graphs
Healthcare Facilities and Services
Morbidity and Mortality
Maternal and Newborn Health
Family Planning
Immunization
Nutrition
Sources
Isalkar, Umesh. 2020. "Dhule’s Popular 'Poor People’s Doctor' Succumbs to Virus." The Times of India, India. timesofindia.indiatimes.com/city/pune/dhules-popular-poor-peoples-doc-succumbs-to-virus/articleshow/77643367.cmshttps://timesofindia.indiatimes.com/city/pun…
James M Campbell. 1880. Gazetteer Of Bombay Presidency: Khandesh, Vol 12. Government Central Press, Bombay.
KVTR Ayurved College. "About Us." KVTR Ayurved College. kvtrayurvedcollege.ac.in/about-us/https://kvtrayurvedcollege.ac.in/about-us/
M Choksi, B. Patil et al. 2016. Health systems in India. Vol 36 (Suppl 3). Journal of Perinatology.https://pmc.ncbi.nlm.nih.gov/articles/PMC514…
Maharashtra State Gazetteers. 1974. Dhulia District. Directorate of Government Printing, Stationery & Publications, Government of Maharashtra, Mumbai.
Mathew George. 2023. The real purpose of the medical college. The Hindu. www.thehindu.com/opinion/op-ed/the-real-purpose-of-the-medical-college/article67232008.ecehttps://www.thehindu.com/opinion/op-ed/the-r…
National Health Mission (NHM). "About Accredited Social Health Activist (ASHA)." National Health Mission, India. nhm.gov.in/index1.php?lang=1&level=1&sublinkid=150&lid=226#:~:text=One%20of%20the%20key%20components,performing%20her%20spelled%20out%20roles.https://nhm.gov.in/index1.php?lang=1&level=1…
Rama Baru. 1999. “Missionaries in Medical Care. Vol. 34, No. 9. Economic and Political Weekly. www.jstor.org/stable/4407696https://www.jstor.org/stable/4407696
Last updated on 26 July 2025. Help us improve the information on this page by clicking on suggest edits or writing to us.