Contents
- Healthcare Infrastructure
- Three-Tiered Structure in the District
- Age-Old Practices & Remedies
- NGOs & Initiatives
- Graphs
- Healthcare Facilities and Services
- A. Public and Govt-Aided Medical Facilities
- B. Private Healthcare Facilities
- C. Approved vs Working Anganwadi
- D. Anganwadi Building Types
- E. Anganwadi Workers
- F. Patients in In-Patients Department
- G. Patients in Outpatients Department
- H. Outpatient-to-Inpatient Ratio
- I. Patients Treated in Public Facilities
- J. Operations Conducted
- K. Hysterectomies Performed
- L. Share of Households with Access to Health Amenities
- Morbidity and Mortality
- A. Reported Deaths
- B. Cause of Death
- C. Reported Child and Infant Deaths
- D. Reported Infant Deaths
- E. Select Causes of Infant Death
- F. Number of Children Diseased
- G. Population with High Blood Sugar
- H. Population with Very High Blood Sugar
- I. Population with Mildly Elevated Blood Pressure
- J. Population with Moderately or Severely High Hypertension
- K. Women Examined for Cancer
- L. Alcohol and Tobacco Consumption
- Maternal and Newborn Health
- A. Reported Deliveries
- B. Institutional Births: Public vs Private
- C. Home Births: Skilled vs Non-Skilled Attendants
- D. Live Birth Rate
- E. Still Birth Rate
- F. Maternal Deaths
- G. Registered Births
- H. C-section Deliveries: Public vs Private
- I. Institutional Deliveries through C-Section
- J. Deliveries through C-Section: Public vs Private Facilities
- K. Reported Abortions
- L. Medical Terminations of Pregnancy: Public vs Private
- M. MTPs in Public Institutions before and after 12 Weeks
- N. Average Out of Pocket Expenditure per Delivery in Public Health Facilities
- O. Registrations for Antenatal Care
- P. Antenatal Care Registrations Done in First Trimester
- Q. Iron Folic Acid Consumption Among Pregnant Women
- R. Access to Postnatal Care from Health Personnel Within 2 Days of Delivery
- S. Children Breastfed within One Hour of Birth
- T. Children (6-23 months) Receiving an Adequate Diet
- U. Sex Ratio at Birth
- V. Births Registered with Civil Authority
- W. Institutional Deliveries through C-section
- X. C-section Deliveries: Public vs Private
- Family Planning
- A. Population Using Family Planning Methods
- B. Usage Rate of Select Family Planning Methods
- C. Sterilizations Conducted (Public vs Private Facilities)
- D. Vasectomies
- E. Tubectomies
- F. Contraceptives Distributed
- G. IUD Insertions: Public vs Private
- H. Female Sterilization Rate
- I. Women’s Unmet Need for Family Planning
- J. Fertile Couples in Family Welfare Programs
- K. Family Welfare Centers
- L. Progress of Family Welfare Programs
- Immunization
- A. Vaccinations under the Maternal and Childcare Program
- B. Infants Given the Oral Polio Vaccine
- C. Infants Given the Bacillus Calmette Guerin (BCG) Vaccine
- D. Infants Given Hepatitis Vaccine (Birth Dose)
- E. Infants Given the Pentavalent Vaccines
- F. Infants Given the Measles or Measles Rubella Vaccines
- G. Infants Given the Rotavirus Vaccines
- H. Fully Immunized Children
- I. Adverse Effects of Immunization
- J. Percentage of Children Fully Immunized
- K. Vaccination Rate (Children Aged 12 to 23 months)
- L. Children Primarily Vaccinated in (Public vs Private Health Facilities)
- Nutrition
- A. Children with Nutritional Deficits or Excess
- B. Population Overweight or Obese
- C. Population with Low BMI
- D. Prevalence of Anaemia
- E. Moderately Anaemic Women
- F. Women with Severe Anaemia being Treated at an Institution
- G. Malnourishment Among Infants in Anganwadis
- Sources
PALGHAR
Health
Last updated on 26 July 2025. Help us improve the information on this page by clicking on suggest edits or writing to us.
Palghar’s healthcare landscape, like many other regions across India, is shaped by a mix of indigenous and Western medical practices. For generations, local communities depended on traditional knowledge passed down through families and village vaidyas, using local herbs, roots, and forest plants to treat common illnesses. Historical records, including entries in the Thane District Gazetteer (1882), provide early glimpses of how government-run dispensaries and health centres began to appear in the area, gradually complementing older systems of healing.
Under British rule, the district’s network of healthcare facilities began to expand and continued to grow after independence through the efforts of local leaders and community groups who worked to bring medical services to remote villages. The establishment of the Rural Health Training Centre in the 1950s, notably, marked an important step in building local capacity, providing care, and training health workers to meet the needs of the district’s rural communities.
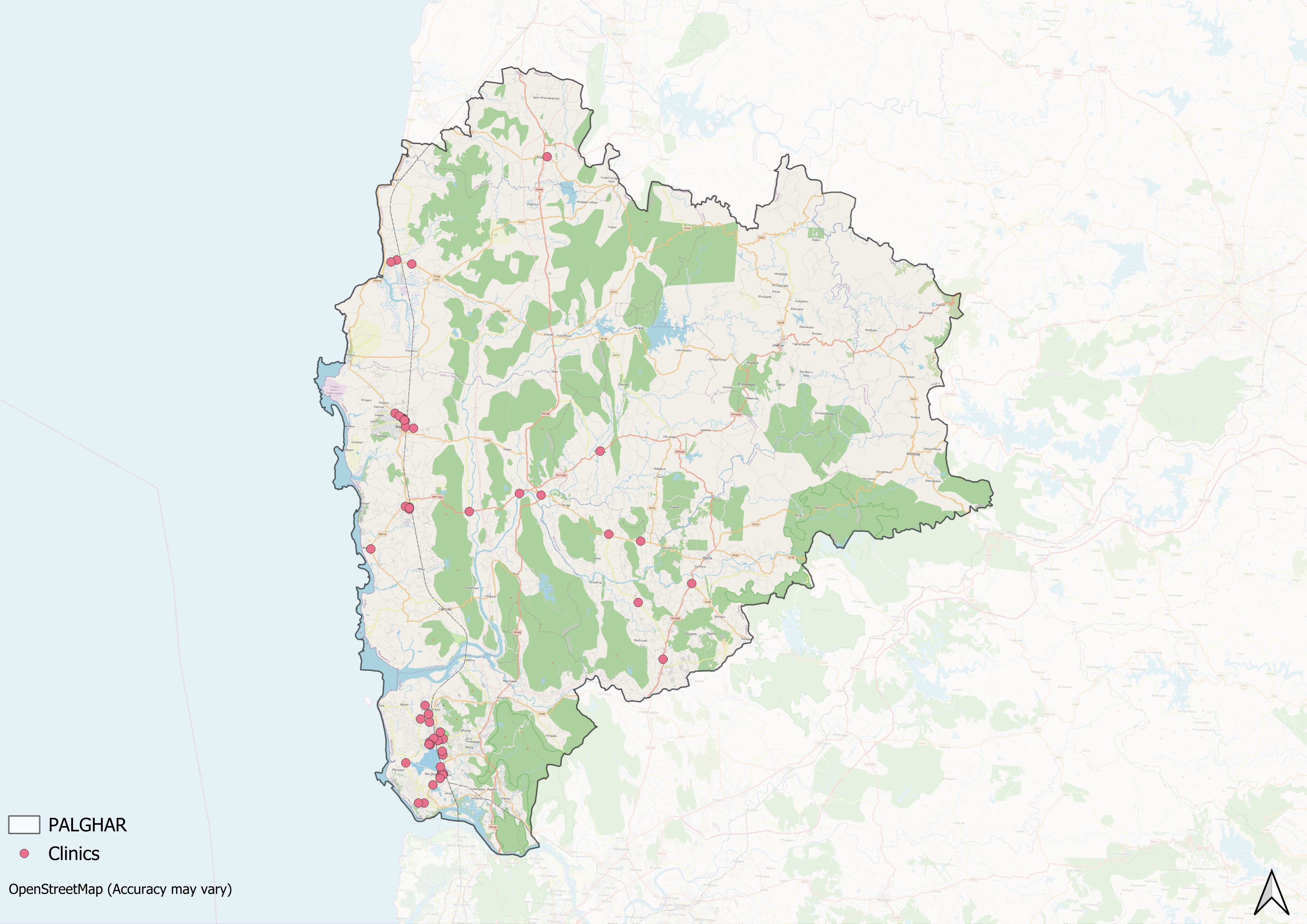
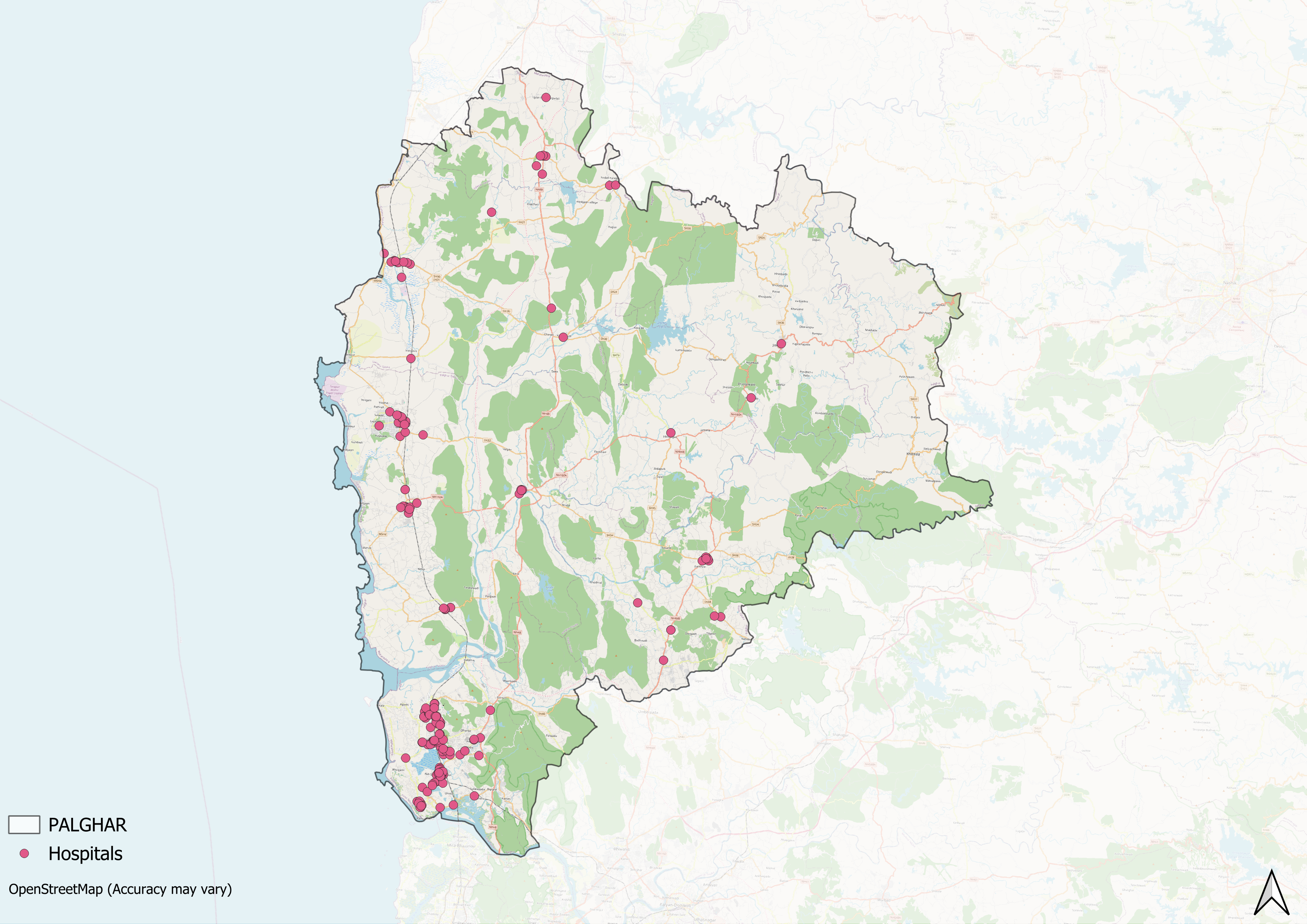
Healthcare Infrastructure
Similar to other regions in India, Palghar’s healthcare infrastructure follows a multi-tiered system that involves both public and private sectors. Currently, the public healthcare system is tiered into primary, secondary, and tertiary levels. Primary care is provided through Sub Centres and Primary Health Centres (PHCs), while secondary care is managed by Community Health Centres (CHCs) and Sub-District hospitals. Tertiary care, the highest level, includes Medical Colleges and District Hospitals. This system has been shaped and refined over time, influenced by national healthcare reforms.
Supporting this network is a large cadre of Accredited Social Health Activists (ASHAs) who, as described by the National Health Mission, serve as “an interface between the community and the public health system.” These frontline workers play a vital role in reaching underserved areas and connecting families to essential services.
Three-Tiered Structure in the District
Palghar district was officially formed on 1 August 2014, carved out of the larger Thane district for more focused governance and administration. Before this, the region fell under the jurisdiction of Thane, and its development often remained overshadowed by its proximity to Mumbai and the industrialised parts of Thane.
Detailed records of the earliest medical services are scarce. However, references from the late nineteenth century suggest that basic healthcare in the area first took shape through government-run dispensaries and rural health centres, similar to arrangements seen elsewhere in Maharashtra during the British period. The Thane District Gazetteer of 1882 provides one such record for Bassein (modern-day Vasai), noting: “The Balvantrav Hari Naik Bassein dispensary, established in 1872, is in bad repair. The prevailing diseases are fevers, worms, rheumatic and respiratory affections, and skin diseases.”
Although close to better-served districts like Mumbai and Thane, Palghar remained underdeveloped in terms of healthcare for many years. This began to change after independence, as residents and community leaders worked to improve health services in the area.
In 1948, Shrimati Ramabai Dandekar took significant steps to address the lack of care for mothers and children. With support from the Bombay Mother and Child Welfare Society, she set up the district’s first nursing care centre, which improved access to basic health services for women and children. She later founded the Mata-Bal Sangopan Kendra, Palghar’s first maternity hospital.
![Shrimati Ramabai Dandekar[1]](/media/statistic/images/maharashtra/palghar/health/shrimati-ramabai-dandekar1-67524f62.png)
The district’s healthcare capacity continued to expand in the decades that followed. In 1956, the Rural Health Training Centre Palghar was opened with support from the Grant Government Medical College and Sir J.J. Group of Hospitals in Mumbai. This centre has served as an important site for providing medical care and training health workers for rural communities.
In 2000, the Rural Homoeopathic Hospital Palghar (formally the Dr. M.L. Dhawale Memorial Trust Hospital) was established to serve the district’s large tribal population. It, notably, became the first homeopathic hospital in Maharashtra to receive NABH accreditation.
![Rural Health Training Center[2]](/media/statistic/images/maharashtra/palghar/health/rural-health-training-center2-62bed1c1.png)
Age-Old Practices & Remedies
Historically, before the advent of Western healthcare systems or the three-tiered healthcare infrastructure that exists today, people in the district relied on and made use of indigenous knowledge and medicine for their well-being. India has long been known for its pluralistic health traditions, and this holds true for Palghar, where indigenous practices have remained deeply rooted in daily life.
In the coastal areas of Dahanu, where many indigenous communities live, traditional knowledge is closely connected with the surrounding forests and natural environment. Local plants gathered from nearby forests form the basis of many home-made remedies. Among the plants commonly used are Gunja (Abrus precatorius L.), Petari (Abutilon indicum L.), and Maranda (Acanthus illicifolius L.).
![Gunja[3]](/media/statistic/images/maharashtra/palghar/health/gunja3-2dfe7cd9.png)
Alongside such plant-based treatments, many villages once had local vaidyas, traditional healers who shared their knowledge within families and communities. Their treatments combined herbal prescriptions with spiritual guidance and rituals, which became part of household routines and beliefs passed down through generations. One well-known Ayurvedic preparation still made in some households is Dashamula Ashite, a simple herbal decoction whose name comes from the Sanskrit for “ten roots.”
Made from a combination of various roots such as Bilva (Aegle marmelos), Agnimantha (Premna serratifolia), Gambhari (Gmelina arborea), Shyonaka (Oroxylum indicum), Patala (Stereospermum suaveolens), Brihati (Solanum indicum), Shalaparni (Desmodium gangeticum), Kantakari (Solanum xanthocarpum), Gokshura (Tribulus terrestris), and Prishnaparni (Uraria picta), it is taken to ease pain, manage inflammation, and treat digestive conditions when used as an enema.
![Bilva[4]](/media/statistic/images/maharashtra/palghar/health/bilva4-fe32531f.png)
NGOs & Initiatives
The determinants of health and health outcomes, as the World Health Organization (WHO) elaborates, are not solely shaped by medical factors and healthcare services. The organization uses the term “social determinants of health (SDH)” to refer to the “non-medical factors that influence health outcomes.” These non-medical factors can be sanitation, nutrition, community well-being, or, as the WHO outlines, “income and social protection,” “food security,” access to quality healthcare, and more.
While there have been ongoing efforts to strengthen Palghar district’s healthcare infrastructure, certain areas still face challenges, particularly in addressing these broader health determinants. In response, non-governmental organizations have emerged as vital partners, working alongside public health systems to develop innovative, grassroots-level approaches that bridge these gaps.
AROEHAN is a non-governmental organisation operating in the Palghar district. Established with the aim of improving health and development outcomes in remote and underserved regions, the organisation focuses primarily on the welfare of indigenous communities residing in Mokhada, Jawhar, and Dahanu blocks.
![A community health awareness session conducted by AROEHAN, engaging women and adolescents from remote villages in Palghar district.[5]](/media/statistic/images/maharashtra/palghar/health/a-community-health-awareness-session-conduct_0X2xvz3.png)
AROEHAN works in close partnership with local communities and government health services to strengthen access to essential healthcare, particularly maternal and child health. The organisation provides medical equipment, supports rural hospitals with diagnostic tools, and has supplied an ambulance to improve emergency transport services in the Mokhada area.
A core part of AROEHAN’s work targets maternal, prenatal, and neonatal health challenges, with a focus on addressing issues such as low birth weight, which is often linked to malnutrition, anaemia, and early pregnancies. The organisation adopts a community-based approach, revitalising Mata Samitis, committees formed under India’s Integrated Child Development Scheme (ICDS), to monitor and support maternal and child health programmes at the village level. To encourage local participation, AROEHAN has conducted hundreds of meetings with these committees and organised frequent Mata Baithaks, informal gatherings where pregnant and nursing mothers receive guidance on topics such as nutrition, immunisation, and maintaining health records.
In addition to maternal health initiatives, AROEHAN also works with adolescents, promoting awareness on subjects such as menstrual health and nutrition. The organisation distributes health tracking diaries to young girls and monitors haemoglobin levels through portable diagnostic devices, aiming to reduce anaemia and build awareness about personal health care among adolescent girls.
Through these programmes, AROEHAN continues to address gaps in healthcare delivery and tackle broader social determinants of health in some of Palghar district’s most remote communities.
Graphs
Healthcare Facilities and Services
Morbidity and Mortality
Maternal and Newborn Health
Family Planning
Immunization
Nutrition
Sources
Annual Report 2020-21, Aroehan, 7-17. aroehan.org/wp-content/uploads/2022/03/AROEHAN-Annual-Report-FY-20-21.pdfhttps://aroehan.org/wp-content/uploads/2022/…
Gazetteer Department, Government of Maharashtra. 1882 (reprinted 1986). Gazetteers of the Bombay Presidency: Thana District (Vol. XIII, Part II).
M Choksi, B. Patil et al. 2016. Health systems in India. Vol 36 (Suppl 3). Journal of Perinatology. pmc.ncbi.nlm.nih.gov/articles/PMC5144115/https://pmc.ncbi.nlm.nih.gov/articles/PMC514…
M. L. Dahanukar Trust. "Palghar Projects." M. L. Dahanukar Trust. mldtrust.org/palghar/https://mldtrust.org/palghar/
National Health Mission (NHM). "About Accredited Social Health Activist (ASHA)." National Health Mission, India. nhm.gov.in/index1.php?lang=1&level=1&sublinkid=150&lid=226#:~:text=One%20of%20the%20key%20components,performing%20her%20spelled%20out%20roleshttps://nhm.gov.in/index1.php?lang=1&level=1…
Rural Health Training Centre, Palghar. "About Us." RHTC Palghar. www.rhtcpalghar.com/aboutus.htmlhttps://www.rhtcpalghar.com/aboutus.html
Shivangi Chaudhari, Dakshata Patil, Jayananda Tosh. 2017. "Traditional Ethnomedicinal Plants Used by the Tribal in the Coastal Area of Dahanu Taluka, Palghar District, Maharashtra State, India." Vol. 13, no. 1. International Journal of Scientific Research (IJSR). www.worldwidejournals.com/international-journal-of-scientific-research-(IJSR)/article/traditional-ethnomedicinal-plants-used-by-the-tribal-in-coastal-area-of-dahanu-taluka-palghar-district-maharashtra-state-india/MTAyMTM=/?is=1https://www.worldwidejournals.com/internatio…
Social determinants of health. WHO. www.who.int/health-topics/social-determinants-of-health#tab=tab_1https://www.who.int/health-topics/social-det…
Last updated on 26 July 2025. Help us improve the information on this page by clicking on suggest edits or writing to us.